Is my baby allergic to my milk?
The short answer is no, babies aren’t allergic to breastmilk itself. However, they can react to certain food proteins present in your milk, such as cows’ milk protein. This condition is known as cows’ milk protein allergy (CMPA), and while it’s the most common food allergy in infants, it’s not actually that common, especially among exclusively breastfed babies. Research suggests that CMPA affects around 2-6% of infants overall, but only about 0.5% of exclusively breastfed babies. This lower prevalence in breastfed infants is attributed to the significantly lower levels of cows’ milk protein present in breastmilk compared to formula milk. There is 100,000 times less cows’ milk protein in breastmilk than in cows’ milk itself. CMPA is more common though in babies that have had infant formula within the first 4 months of life.
Research suggests that CMPA affects around 2-6% of infants overall, but only about 0.5% of exclusively breastfed babies.
Identifying CMPA symptoms
CMPA symptoms can be broad and may overlap with other issues, making diagnosis challenging. The symptoms can manifest in various bodily systems, including the digestive system, skin, and respiratory system. Common symptoms include fussiness, reflux, colic, digestive discomfort, changes in stool consistency, and skin rashes. However, it’s essential to note that not all babies with CMPA will display all of these symptoms.
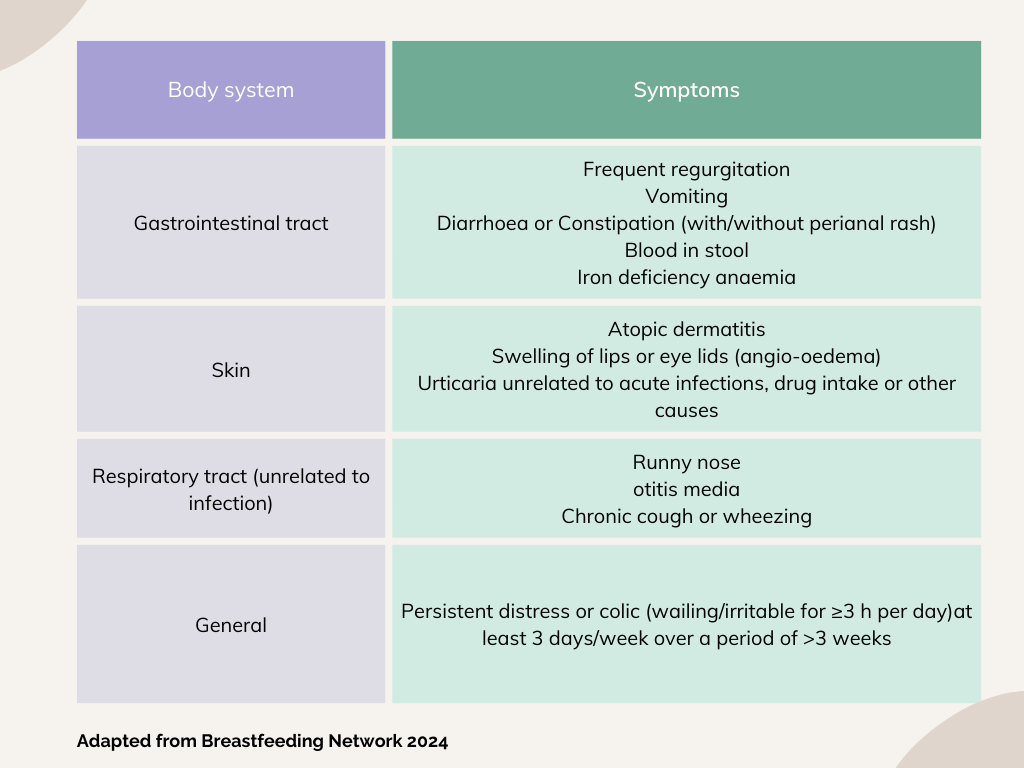
Symptoms vary from baby to baby and symptoms may vary in severity. Part of getting a correct diagnosis of CMPA is about correctly identifying the root cause of these symptoms and addressing this to ensure you and your baby are getting the correct management and treatment. Many infant feeding issues can result in similar symptoms, so before a diagnosis of CMPA is assumed, infant feeding should be assessed by a qualified practitioner.
Types of CMPA
There are two main classifications of CMPA: Immunoglobulin-E (IgE) mediated allergy and Non-Immunoglobulin-E mediated allergy (Non-IgE).
IgE-mediated allergy typically results in immediate reactions, such as hives, swelling, vomiting, or difficulty breathing, occurring shortly after ingesting the allergen, usually within 2 hours but can be withing minutes. Cows’ milk protein peaks in concentration in your breast milk around an hour after you have ingested it. This type of allergy is caused by an over-reaction of the immune system, causing lots of inflammation. Reactions can vary from mild to severe, in some cases anaphylaxis can occur and this is potentially life threatening. You will be pleased to know this type of reaction is rare in infants (but you should seek immediate medical help if your baby has any symptoms such as difficulty breathing or swelling to their face/mouth).
Non-Immunoglobulin-E mediated allergy reactions are more delayed, so may take longer to appear. It could be 72 hours later, sometimes even up to a week. Symptoms such as delayed skin rashes and gastrointestinal issues, tend to be more common. (Sub categories of this type of allergy such as FPIES can result in vomiting and a quicker occurrence of symptoms). This type of delayed allergy often, and mistakenly gets labelled as an intolerance, but this isn’t correct. It is still an allergy. The immune system is still involved.
This can make it very tricky to pinpoint what is causing this reaction. This extended length of time before a reaction occurs can make it difficult to see the correlation. If your baby is unsettled, ‘fussy’, has some looser stools you may not link that to something you have eaten a good few days before. This can result in you continuing to ingest the cows’ milk protein before identifying this is the root cause of your baby’s symptoms.

Breastfeeding with CMPA
You can continue to breastfeed if your baby has CMPA. In fact, is recommended to keep breastfeeding if you can. Breastmilk provides numerous benefits, including anti-inflammatory properties that can help alleviate your baby’s symptoms and help repair any inflammation and damage caused by the allergic reaction.
Historically parents have been given incorrect information to stop breastfeeding if their baby was thought to have an allergy, and this is not necessary. However, if breastfeeding is not possible or you are combination feeding, specialised hypoallergenic formulas will be needed. These formulas contain proteins that are broken down into smaller, less allergenic fragments, making them easier for sensitive infants to tolerate. Breastmilk however still contains less concentration of cows’ milk protein than these formulas. Remember if your baby is having formula but you want to continue to breastfeed you need to express to maintain your breastmilk supply.
Historically parents have been given incorrect information to stop breastfeeding if their baby was thought to have an allergy, and this is not necessary.
Diagnosing CMPA
Diagnosing CMPA can be complex and should involve a thorough evaluation of the baby’s symptoms, medical history, and family history of allergies. An elimination diet is the main way to confirm a diagnosis of CMPA. There can be incorrect information given to families about how to do this. It is a myth that it takes weeks for the cows’ milk protein to leave your breastmilk.
Many families have been incorrectly informed that you have to remove dairy for at least 6 weeks for the protein to leave your milk and to see any improvement. Generally, it has left your breastmilk within 24 hours after ingestion. You do not have to switch to formula, stop breastfeeding or wait weeks and weeks to confirm the diagnosis of CMPA. 1-2 weeks of removing dairy should demonstrate an improvement in symptoms. This may not be a full resolution of all symptoms, but if your baby is reacting to cows’ milk and you remove it from your diet, you should see some positive changes, usually within 5-7 days. It may take longer for gut inflammation to reduce and so some symptoms (such as excess mucus or blood in stool, a rash) can take longer to improve, so it may be recommended you remove diary (all dairy) from your diet for a minimum of 2 weeks.
Additionally, skin prick tests or blood tests may be conducted to assess for IgE-mediated allergies. But, these are not always accurate in babies under 6 months of age, and do not confirm the presence of a Non mediated IgE allergy. This can only be confirmed by the elimination of dairy from your diet. Most babies tend to have a Non- IgE mediated type allergy and the good news is that the majority of babies with this type of allergy have outgrown it by the age of three (often even earlier).
Managing CMPA
If CMPA is diagnosed, the primary treatment is eliminating cows’ milk protein from the baby’s diet. For breastfeeding parents, this means avoiding dairy products while continuing to breastfeed. You will need a Vitamin D and Calcium supplement whilst you are following a dairy free diet (link here to guidance on this? Breastfeeding a Baby with CMA | The GP Infant Feeding Network (UK) (gpifn.org.uk)).
It is often suggested, just give up dairy, but this is not always that simple. There can be hidden dairy in foods, eating out, slip ups will happen and you may intentionally eat dairy because you are really missing it, then feel awful if this results in your baby getting symptoms again following this. If you do consume some dairy, it can be useful to note down any response/symptoms that show in your little one, look at it as information. How quickly did the symptoms show, how quickly did they go? Were they the same as before or different? It’s all good information!

Reintroducing dairy
Once CMPA symptoms have resolved, the gradual reintroduction of dairy into your or your baby’s diet (if they are eating solids) may be considered. The current recommendations for this are 6 months from the confirmation of CMPA and when your baby is around 9-12 months of age. This process typically involves following a step-by-step approach outlined in guidelines known as iMAP guidance, also often referred to as the milk ladder. However, it’s essential to proceed with caution and monitor your baby for any recurrence of symptoms.
Once CMPA symptoms have resolved, the gradual reintroduction of dairy into your or your baby’s diet (if they are eating solids) may be considered.
Seeking support for CMPA
Managing CMPA can be overwhelming, especially when navigating dietary restrictions and trying to interpret your baby’s symptoms. Seeking support from the right health care professionals, knowledgeable about CMPA is important to help you navigate this. Lactation consultants, your GP, a Paediatrician and dietitian (if a referral is necessary), can provide valuable guidance and reassurance to help you on this journey. Additionally, connecting with other parents who have experience managing CMPA can offer emotional support and practical tips for coping with the challenges. There are some links to additional useful guidance included below.
Conclusion
Cows’ milk protein allergy (CMPA) can present challenges for breastfeeding parents. With the correct information, proper understanding, support, and management, it is possible to continue breastfeeding successfully while addressing yours and your baby’s nutritional needs and managing their symptoms effectively. Working closely with healthcare professionals and being proactive in seeking support, can help you navigate CMPA with confidence, ensuring the best possible outcomes for your baby and the longevity of your breastfeeding journey.
References
- Emmert V, Lendvai-Emmert D, Eklics K, Prémusz V, Tóth GP. Current Practice in Pediatric Cow’s Milk Protein Allergy-Immunological Features and Beyond. Int J Mol Sci. 2023 Mar 6;24(5):5025. doi: 10.3390/ijms24055025. PMID: 36902457; PMCID: PMC10003246.
- BMJ 2018; 363 doi: https://doi.org/10.1136/bmj.k5056 (Published 05 December 2018)Cite this as: BMJ 2018;363:k5056
- BMJ 2013; 347 doi: https://doi.org/10.1136/bmj.f5424 (Published 16 September 2013)Cite this as: BMJ 2013;347:f5424
- Cow’s milk allergy in children | Health topics A to Z | CKS | NICE
- What is FPIES? – The FPIES Foundation
- Nuzzi G, Di Cicco ME, Peroni DG. Breastfeeding and Allergic Diseases: What’s New? Children (Basel). 2021 Apr 24;8(5):330. doi: 10.3390/children8050330. PMID: 33923294; PMCID: PMC8145659.
- Foong RX, du Toit G, Fox AT. Asthma, Food Allergy, and How They Relate to Each Other. Front Pediatr. 2017 May 9;5:89. doi: 10.3389/fped.2017.00089. PMID: 28536690; PMCID: PMC5422552.
- Yakaboski E, Robinson LB, Arroyo A, et al. Early introduction of food allergens and risk of developing food allergy. Nutrients. 2021;13(7):2318. doi:10.3390/nu13072318
- Cows’ Milk Allergy | The GP Infant Feeding Network (UK) (gpifn.org.uk)
Useful links
Cows Milk Protein Allergy (CMPA) and Breastfeeding.pdf (breastfeedingnetwork.org.uk)