The Academy of Breastfeeding Medicine (ABM) recognizes that the shortage of breastmilk substitutes (infant formula) has reached critical levels in some areas and recommends the following in order to help support the safety and health of mothers, infants, and children until such a time as the crisis averts:
For those CURRENTLY PREGNANT or EXPECTING A BABY:
- Consider potential infant formula shortages and risks when making your decisions and plans about infant feeding. Seek prenatal breastfeeding education, and connect with health care providers and hospitals that are supportive of breastfeeding.
For those CURRENTLY NOT BREASTFEEDING or CURRENTLY NOT MAKING ANY BREAST MILK:
- Consider re-lactating. Re-lactating is the process by which a person who has given birth may ramp-up milk production after a period of not lactating or partially lactating.1–4 (Note, seek consultation with a skilled lactation provider and/or expert in Breastfeeding Medicine if you plan to try to re-lactate. This may be a challenging process for some, especially the further out one gets from birth.)
- Consider pasteurized donor human milk from a certified human milk bank if you have the means and availability to purchase.
- If you are considering using anyone’s breastmilk other than your own, consider safety and ensure informed decision making that considers the potential risks and benefits, and consider donor screening and flash pasteurization.5 Wet nursing, and close family members and friends breastfeeding is a way in which some societies and cultures have fed infants historically and in modern day. (Note, this should only be done with trusted family members and friends, and ideally the donor would have had testing to make sure they were free of any transmissible diseases.)
- Avoid use of “home” recipes for making your own formula unless you have consulted first with your baby’s doctor.
- Do not mix the formula in any way other than how it is written on the package instructions as these practices can have severe, at times fatal consequences for the infant.
- Avoid feeding your baby younger than one year of age regular cow’s milk as it can lead to serious consequences such as iron deficiency which can harm cognitive development. (Note, in an emergency, for infants 6 months to 1 year of age, cow’s milk may be used for a short time {on the order of days.} This is considered safer than diluting or making homemade formula. Consult your baby’s doctor if you have to give your baby cow’s milk under one year of age as they will need to monitor your baby’s iron status.)
- You can transition from one brand of formula to another if that is all you have access to. (Note, if your infant is on a special formula for a medical condition, speak with your baby’s doctor and/or a pediatric nutritionist before making any substitutions.)
- Do not purchase breastmilk or infant formula on the internet from anyone or any source that you are not familiar with and can completely trust. Consider your resources for safely ordering and shipping from a trusted source. Seek assistance from a local breastfeeding professional.
- Place only the amount that your baby will eat in the bottle, so as not to waste any of your supply.
- Talk with your baby’s doctor about the timing and appropriateness of introducing solid foods no more than 2-3 times/day in place of a bottle feeding.
- Do not give your baby under 6 months of age any water, tea, or juice.
For those CURRENTLY PARTIALLY BREASTFEEDING:
- Consider transitioning back to full breastfeeding while the shortage remains. This is healthy for your infant and also will help lessen some of the demand on the current supply. (Note, if you need help with increasing your production, seek consultation with a skilled lactation provider and/or an expert in Breastfeeding Medicine. 1–4 We recommend you speak with your baby’s healthcare provider because you will likely need to do this gradually as your milk production increases. Your baby’s provider can monitor your baby’s growth to make sure it stays on target.)
- Consider pasteurized donor human milk from a certified human milk bank if you have the means and availability to purchase.
- Avoid use of “home” recipes for making your own formula unless you have consulted first with your baby’s doctor.
- If you are considering using anyone’s breastmilk other than your own, consider safety and ensure informed decision making that considers the potential risks and benefits, and consider donor screening and flash pasteurization.5 Wet nursing, and close family members and friends breastfeeding is a way in which some societies and cultures have fed infants historically and in modern day. (Note, this should only be done with trusted family members and friends, and ideally the donor would have had testing to make sure they were free of any transmissible diseases.)
- Do not mix the formula in any way other than other than how it is written on the package instructions as these practices can have severe, at times fatal consequences for the infant.
- Avoid feeding your baby younger than one year of age regular cow’s milk as it can lead to serious consequences such as iron deficiency which can harm cognitive development. (Note, in an emergency, for infants 6 months to 1 year of age, cow’s milk may be used for a short time {on the order of days.} This is considered safer than diluting or making homemade formula Consult your baby’s doctor if you have to give your baby cow’s milk under one year of age as they will need to monitor your baby’s iron status.)
- You can transition from one brand of formula to another if that is all you have access to. (Note, if your infant is on a special formula for a medical condition, speak with your baby’s doctor and/or a pediatric nutritionist before making any substitutions.)
- Do not purchase breastmilk or infant formula on the internet from anyone or any source that you are not familiar with and can completely trust. Consider your resources for safely ordering and shipping from a trusted source. Seek assistance from a local breastfeeding professional.
- When feeding your infant, place only the amount that your baby will eat in the bottle, so as not to waste any of your supply.
- Talk with your baby’s doctor about the timing and appropriateness of introducing solid foods no more than 2-3 times/day in place of a bottle feeding.
- Place only the amount that your baby will eat in the bottle, so as not to waste any of your supply.
- For premature babies, if you are using the formula only to fortify your breastmilk and your baby is growing well, talk with your baby’s doctor about the need to continue fortification and/or do a trial with just your breast milk.
- Do not give your baby under 6 months of age any water, tea, or juice.
For those CURRENTLY EXCLUSIVELY BREASTFEEDING:
- Consider donating your excess milk to a local milk bank that is certified by the Human Milk Banking Association of North America (HMBANA) or similar organization.
- Consider increasing your supply in order to produce more than your baby needs in order to be able to donate any excess milk to a local milk bank that is certified by the Human Milk Banking Association of North America (HMBANA) or similar organization.
For HEALTH CARE PROFESSIONALS:
- Be sure you are consulting and accessing the most recent, evidence-based recommendations. Formula supplementation should be reserved only for medical indications.6,7
- Take the current formula shortage into account when counseling families to make important feeding decisions for their babies. Give them accurate information about the risks and benefits of formula feeding so they can make a true, informed choice.
- Support the families who desire to breastfeed by providing them with adequate anticipatory guidance and support about what to do and how to access help if they encounter any difficulties in order to help them avoid the steep drop-off of breastfeeding in the early days.
- Access the Academy of Breastfeeding Medicine’s evidence-based clinical protocols related to breastfeeding, human milk, and lactation at www.bfmed.org/protocols.
- Familiarize yourself with local breastfeeding and lactation professionals such as International Board Certified Lactation Consultants (IBCLC’s) or doctors with expertise in Breastfeeding Medicine.
For COMMUNITIES, SOCIETIES, AND GOVERNMENTS:
- Start making plans now to help avoid a crisis such as this in the future by putting in place structural, systemic resources and supports for all expectant and new families to decrease the need for unnecessary supplementation of breastfeeding infants.
- Implement universal policies and practices to ensure that all mothers are able to reach their personal breastfeeding goals such as evidence-based in-hospital support for breastfeeding families that adheres to the Ten Steps to Successful Breastfeeding8, paid maternity and family leave, workplace support for breastfeeding and milk expression, and access and coverage for professional breastfeeding and lactation care.
- Improve monitoring and regulation of direct marketing of breastmilk substitutes to consumers and healthcare professionals and fully-adopt the International Code of Marketing of Breast-Milk Substitutes.9–11
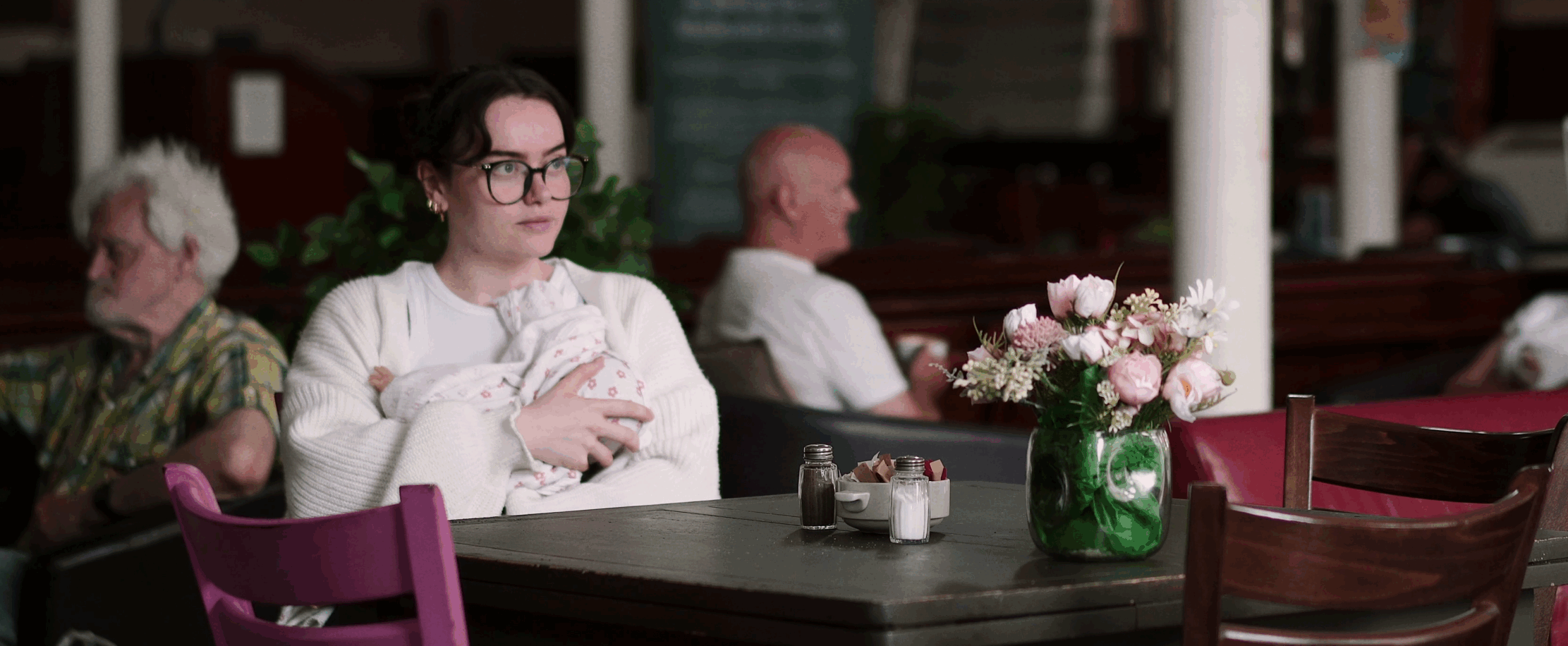
- Ensure public spaces visibly and actively support mothers breastfeeding their infants.
Ann Kellams, MD, IBCLC, FAAP, FABM on behalf of the Academy of Breastfeeding Medicine.
The Academy of Breastfeeding Medicine (ABM) is a global organization of medical doctors with over 1,000 members whose mission is to educate and empower health professionals to support and manage breastfeeding, lactation, and human milk feeding in order to achieve healthier lives worldwide through excellence in the medical care of breastfeeding and lactation. We curate, support, and share high-quality research and innovative solutions and strive to ensure that professionals are enabled to support and nurture families with safe and effective care. www.bfmed.org
- Piovanetti Y, Calderon C, Budet Z, Aparicio RJ, Rivera Rios MV. Breastfeeding, a Vital Response in Emergencies. Pediatrics. February 2022.
- In a Natural Disaster or Public Health Emergency. https://publications.aap.org/DocumentLibrary/Solutions/PCO/FormsTools/disasterfactsheet.pdf. Accessed May 16, 2022.
- Disaster Planning: Infant and Child Feeding | DNPAO | CDC. https://www.cdc.gov/nccdphp/dnpao/features/disasters-infant-feeding/index.html. Accessed May 16, 2022.
- Brodribb W. ABM clinical protocol #9: use of galactogogues in initiating or augmenting maternal milk production, second revision 2018. Breastfeed Med. 2018;13(5):307-314. doi:10.1089/bfm.2018.29092.wjb
- Sriraman NK, Evans AE, Lawrence R, Noble L, Academy of Breastfeeding Medicine’s Board of Directors. Academy of breastfeeding medicine’s 2017 position statement on informal breast milk sharing for the term healthy infant. Breastfeed Med. 2018;13(1):2-4. doi:10.1089/bfm.2017.29064.nks
- Kellams A, Harrel C, Omage S, Gregory C, Rosen-Carole C. ABM clinical protocol #3: supplementary feedings in the healthy term breastfed neonate, revised 2017. Breastfeed Med. 2017;12:188-198. doi:10.1089/bfm.2017.29038.ajk
- Feldman-Winter L, Kellams A, Peter-Wohl S, et al. Evidence-Based Updates on the First Week of Exclusive Breastfeeding Among Infants ≥35 Weeks. Pediatrics. 2020;145(4). doi:10.1542/peds.2018-3696
- Ten Steps to Successful Breastfeeding – UNICEF/WHO Baby-Friendly Hospital Initiative (BFHI). http://www.tensteps.org/. Accessed January 19, 2018.
- The International Code of Marketing of Breastmilk Substitutes – Baby Friendly Initiative. https://www.unicef.org.uk/babyfriendly/baby-friendly-resources/international-code-marketing-breastmilk-substitutes-resources/the-code/. Accessed May 16, 2022.
- Maternal, Newborn, Child and Adolescent Health and Ageing Department. https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/formula-milk-industry. Accessed May 16, 2022.
- Scope and impact of digital marketing strategies for promoting breastmilk substitutes. https://www.who.int/publications/i/item/9789240046085. Accessed May 16, 2022.